

One of the most common indicators of a fractured heel bone is tenderness in the area that causes pain, even with slight pressure. Swelling in the foot and ankle area is another prevalent symptom, often accompanied by visible bruising. Individuals with heel fractures usually find it impossible to bear weight on the affected foot, leading to significant mobility limitations. The diagnosis of heel bone fractures typically involves X-rays and computed tomography, or CT, scans. X-rays can provide a clear image of the injury, but in more complex cases, CT scans may be used to obtain a detailed, three dimensional view of the affected area. Non surgical treatment involves protecting the fractured area with a splint, resting the foot by avoiding weight-bearing, and using crutches. Once swelling subsides, a podiatrist may apply a cast to stabilize the fracture. Surgical intervention may be necessary when the fracture affects the joint. It is important to avoid putting any weight on the injured heel until the fracture has fully healed, which may take several months. If you believe you have fractured your heel bone, it is suggested that you make an appointment with a podiatrist.
Many people suffer from bouts of heel pain. For more information, contact Dr. Alan J. Spector of Shore Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our office located in Point Pleasant, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Have you ever gotten up from a chair or out of bed in the morning, and upon taking that first step, feel like your heel has stepped on a tack? Many people experience a feeling of sharp pain which radiates into their arch from their heel and which does not allow them to put their heel on the floor. Sometimes they need to sit back down, stand only on their toes and use the wall for balance. If you can take a few steps, it seems to go away and lessen, allowing you to then resume your activity. Later, throughout your day and after a period of rest, it can happen again. If this sounds familiar you may be suffering from your first attack of heel pain.
Heel pain is a debilitating condition that affects day to day activities. Running and walking both causes stress on the heel because the heel is the part of the foot that hits the ground first. This means that the heel is taking on your entire weight. Diagnosis and treatments for heel pain can be easily found through your podiatrist.
Plantar Fasciitis
One of the main causes of heel pain is a condition known as plantar fasciitis. The plantar fascia is a band of tissue that extends along the bottom of the foot, from the toe to the bottom of the heel. A rip or tear in this ligament can cause inflammation of these tissues, resulting in heel pain. People who do not wear proper fitting shoes are often at risk of developing problems such as plantar fasciitis. Unnecessary stress from ill-fitting shoes, weight change, excessive running, and wearing non-supportive shoes on hard surfaces are all causes of plantar fasciitis.
Achilles Tendonitis
Achilles tendonitis is another cause of heel pain. Similar to plantar fasciitis, inflammation of the Achilles tendon will cause heel pain due to stress fractures and muscle tearing. A lack of flexibility of the ankle and heel is an indicator of Achilles tendonitis. If left untreated, this condition can lead to plantar fasciitis and cause even more pain on your heel.
Heel Spur
A third cause of heel pain is a heel spur. A heel spur occurs when the tissues of the plantar fascia undergo a great deal of stress, leading to a separation of the ligament from the heel bone entirely. This results in a pointed fragment of bone on the ball of the foot, known as a heel spur.
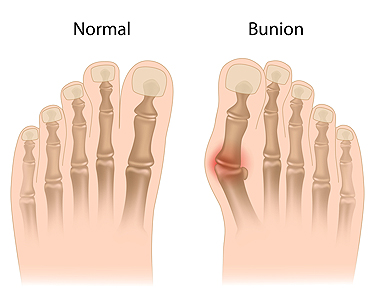
A bunion, medically termed hallux valgus, is a prominent, bony protrusion at the base of the big toe. Often, the only indicator of a mild bunion is its physical manifestation. However, it can also result in discomfort, swelling, and alterations in the foot's structure. In extreme instances, surgical intervention might be necessary due to related issues. Key visual indicators of a bunion are the big toe deviating toward the other toes, forming an outward bulge on the first foot bone. Additionally, there may be a raised bony bump on the foot's exterior, tough skin under the big toe, and calluses on the adjacent toe. Over time, the foot's form may drastically change, impacting both the big toe and other foot regions, making shoe selection challenging. Resulting structural modifications can cause pain, swelling, and bursitis, which is an inflammation of the toe joint's cushioning sac. Some people may face mobility issues with their big toe, affecting their walking. While many individuals do not encounter severe problems from bunions, if left untreated, complications such as arthritis in the big toe or deformities in the adjacent toe can arise. If you have a painful bunion, it is suggested that you make an appointment with a podiatrist who can intervene and help prevent severe complications.
If you are suffering from bunions, contact Dr. Alan J. Spector of Shore Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
If you have any questions, please feel free to contact our office located in Point Pleasant, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions are large bony bumps at the base of the big toe. Medically known as hallux valgus, a bunion is a misalignment of the metatarsophalangeal joint, or big toe joint. The misalignment will generally worsen with time if left untreated.
The exact cause of bunions is unknown, with genetics seen as a potential cause. High heels and poorly-fitted footwear, rheumatoid arthritis, and heredity all seem to be potential factors behind the exacerbation of bunions. Women have been found to be more likely to develop bunions in comparison to men.
Bunions do not always produce symptoms. The best way to tell is if the big toe is pushing up against the next toe and there is a large protrusion at the base of the big toe. You may or may not feel pain. Redness, swelling, and restricted movement of the big toe may be present as well.
Podiatrists use a variety of methods to diagnose bunions. If there are symptoms present, podiatrists will first consider that it is a bunion. If not, a physical examination will be conducted to check function of the big toe. Finally, an X-ray may be taken to view the extent of the bunion and confirm it is a bunion.
Typically, nonsurgical methods are used to treat bunions, unless the bunion has become too misaligned. Orthotics, icing and resting the foot, roomier and better fitted shoes, taping the foot, and pain medication are usually utilized first. If the bunion doesn’t go away or causes extreme pain, surgery may be required. Surgeons will either remove part of the swollen tissue or bone to straighten the toe out.
If you have a bunion, it is recommended to see a podiatrist. The longer it is left untreated, the worse it may get. Podiatrists can properly diagnose and treat a bunion before it gets worse.
Heel pain, often attributed to plantar fasciitis, is a frequent complaint that affects individuals of all ages and activity levels. The plantar fascia, a thick band of tissue that supports the arch of the foot, can become inflamed and damaged, leading to persistent discomfort. Plantar fasciitis typically manifests as sharp, stabbing pain in the heel, particularly with the first steps in the morning or after long periods of rest. This pain often eases with activity but can return after periods of standing or walking. The condition is usually a result of repetitive strain, such as excessive use, which leads to micro-tears in the plantar fascia. Addressing heel pain and plantar fasciitis often involves a multi-faceted approach. Understanding the causes and treatment options for heel pain and plantar fasciitis is the first step in finding relief from this common, yet manageable, foot ailment. If you are experiencing persistent heel pain, it is suggested that you speak to a podiatrist who can determine the most appropriate approach to treating plantar fasciitis.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Alan J. Spector from Shore Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
How Can It Be Treated?
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Point Pleasant, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.

Corns and calluses are skin conditions that result from excess pressure or friction on the feet. A common cause of corns and calluses is wearing ill-fitting shoes, particularly high heels. Tight or uncomfortable footwear, not wearing socks with shoes, and engaging in activities that involve repetitive movements, can result in the formation of corns and calluses. If a corn or callus becomes infected, treatment options include taking antibiotics. Symptoms are redness, warmth, swelling, or discharge. In such cases, a podiatrist can prescribe medication to combat the infection. In the case of stubborn corns or calluses, a podiatrist can offer a range of treatments. Included are debridement to remove the hardened skin and adding padding and insoles to redistribute pressure. In certain situations, custom orthotic devices may be prescribed to address structural issues, and topical medications may be applied to soften the affected area. Prevention of corns and calluses on the feet involves wearing properly fitting shoes and addressing any underlying foot problems. If you need help dealing with problematic corns or calluses on the feet, it is suggested that you make an appointment with a podiatrist.
Corns can make walking very painful and should be treated immediately. If you have questions regarding your feet and ankles, contact Dr. Alan J. Spector of Shore Podiatry. Our doctor will treat your foot and ankle needs.
Corns: What Are They? And How Do You Get Rid of Them?
Corns are thickened areas on the skin that can become painful. They are caused by excessive pressure and friction on the skin. Corns press into the deeper layers of the skin and are usually round in shape.
Ways to Prevent Corns
There are many ways to get rid of painful corns such as:
Treating Corns
Although most corns slowly disappear when the friction or pressure stops, this isn’t always the case. Consult with your podiatrist to determine the best treatment option for your case of corns.
If you have any questions please feel free to contact our office located in Point Pleasant, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
A corn is a lesion that forms in the skin of the foot, and it is typically circular in shape, small in size, and thick and rough in texture. A corn generally occurs as a result of repeated pressure on the skin; one example of this is the rubbing of a shoe against the skin. Corns differ from calluses in that their central cores are harder in texture.
A corn is a relatively common condition with a wide variety of treatment options. If a corn becomes overly uncomfortable or painful, consult with your podiatrist; he can determine the best method of treatment that is appropriate for you. Corns may return if the underlying cause of its development is not treated or removed. Avoid removing corns at home, as improper removal may cause infection.
A callus, similar to a corn, is an area of skin that has become thickened due to repeated pressure and rubbing. The rubbing causes the skin to create a layer of protective skin, which is the formed callus. Calluses can differ in size between people, and they can also become painful.
Multiple treatments are available for calluses. At-home treatment and removal should be avoided, as this can potentially lead to infection. Your podiatrist can best determine the cause of your calluses and suggest the treatment most appropriate for you.

Athlete's foot, scientifically known as tinea pedis, is a fungal infection that can affect anyone. It is notorious for causing discomfort, itching, and unsightly skin changes. Athlete’s foot tends to be more prevalent among older adults, especially males. The primary cause is dermatophytes, a type of fungus that thrive in warm and humid environments. You can contract athlete's foot by walking barefoot on wet and contaminated floors, especially in public areas like locker rooms, showers, and pools. It also can be transmitted by sharing towels, clothing, or shoes with someone who has the infection. Prolonged use of sweaty, tight shoes that create a moist environment for fungi to flourish also increases the risk of infection. Symptoms of athlete's foot can include red and inflamed skin, persistent itchiness, flaky and scaly skin, thickened skin, and dry feet. In severe cases, tiny red blisters may develop between the toes or on the soles of the feet. The good news is that athlete's foot is generally easy to treat with prescribed antifungal creams or oral medications. If you suspect you have a particularly troublesome case of athlete's foot, it is suggested that you make an appointment with a podiatrist for help managing this fungal infection.
Athlete’s Foot
Athlete’s foot is often an uncomfortable condition to experience. Thankfully, podiatrists specialize in treating athlete’s foot and offer the best treatment options. If you have any questions about athlete’s foot, consult with Dr. Alan J. Spector from Shore Podiatry. Our doctor will assess your condition and provide you with quality treatment.
What Is Athlete’s Foot?
Tinea pedis, more commonly known as athlete’s foot, is a non-serious and common fungal infection of the foot. Athlete’s foot is contagious and can be contracted by touching someone who has it or infected surfaces. The most common places contaminated by it are public showers, locker rooms, and swimming pools. Once contracted, it grows on feet that are left inside moist, dark, and warm shoes and socks.
Prevention
The most effective ways to prevent athlete’s foot include:
Symptoms
Athlete’s foot initially occurs as a rash between the toes. However, if left undiagnosed, it can spread to the sides and bottom of the feet, toenails, and if touched by hand, the hands themselves. Symptoms include:
Diagnosis and Treatment
Diagnosis is quick and easy. Skin samples will be taken and either viewed under a microscope or sent to a lab for testing. Sometimes, a podiatrist can diagnose it based on simply looking at it. Once confirmed, treatment options include oral and topical antifungal medications.
If you have any questions, please feel free to contact our office located in Point Pleasant, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.