

Athlete's foot, or tinea pedis, is a fungal infection that affects up to 70 percent of the population. Despite its name, athlete’s foot is not limited to athletes. It can affect anyone exposed to various fungi that thrive in warm and moist environments, such as gyms, locker rooms, swimming pools, and communal showers. Exposure is also possible at nail salons and through contact with contaminated socks, towels and clothing. Direct person-to-person transmission is also possible. Walking barefoot in areas frequented by someone with athlete's foot is a common mode of transmission. Warmth combined with moisture is a popular breeding ground for fungal infections like athlete’s foot. Several factors increase the risk of developing this annoying condition. Walking barefoot in wet, dark areas and wearing footwear made of material that does not breathe create an ideal environment for fungal growth. Excessive sweating or exposure to external moisture increases the risk. Wearing the same shoes and socks for extended periods can damage the skin and leave you open to infection. Individuals with diabetes are predisposed, and having eczema may contribute. Athlete's foot appears to affect more men than women. Pedicures performed in contaminated environments also can contribute to the spread of the disease. If you have been infected with athlete’s foot that has become problematic, it is suggested that you schedule an appointment with a podiatrist for an examination and advanced treatment measures.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet and ankles, contact Dr. Alan J. Spector from Shore Podiatry. Our doctor will treat your foot and ankle needs.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact our office located in Point Pleasant, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Athlete’s foot is a type of fungal infection that affects the skin on the feet. It is caused when the tinea fungus grows on the foot. It is possible to catch the fungus through direct contact with someone who has it or by touching a surface that is contaminated with it. This type of fungus thrives in warm, moist environments such as showers, locker room floors, and swimming pools. Your risk of getting it may also increase by wearing tight-fitting, closed-toe shoes, or by having sweaty feet.
Symptoms of athlete’s foot include itching, stinging or burning sensations between the toes. You may also experience toenails that are discolored, thick, crumbly, or toenails that pull away from the nail bed.
Your podiatrist may diagnose athlete’s foot by detecting these symptoms or by doing a skin test to see if there is a fungal infection present. The most common exam used to detect Athlete’s foot is a skin lesion potassium hydroxide exam. To use this method, your doctor will scrape off a small area of the infected skin and place it into potassium hydroxide. The potassium hydroxide will destroy the normal cells and leave the fungal cells untouched so that they are visible under a microscope.
There are a variety of treatment options for athlete’s foot. Some medications are miconazole (Desenex), terbinafine (Lamisil AT), clotrimazole (Lotrimin AF), butenafine (Lotrimin Ultra), and tolnaftate (Tinactin). While these options may be able to treat your fungus, it is best that you consult with a podiatrist in order to see which treatment option may work best for you.
In some cases, Athlete’s foot may lead to complications. A severe complication would be a secondary bacterial infection which may cause your foot to become swollen, painful, and hot.
There are ways that you can prevent athlete’s foot. Washing your feet with soap and water each day and drying them thoroughly is an effective way to prevent infections. You also shouldn’t share socks, shoes, or towels with other people. It is crucial that you wear shower sandals in public showers, around swimming pools, and in other public places. Additionally, you should make sure you wear shoes that can breathe and change your socks when your feet become sweaty. If you suspect that you have Athlete’s foot, you should seek help from a podiatrist as soon as possible.

Embarking on a running journey is not only invigorating but also demands a proactive approach to prevent injuries and ensure a sustained passion for the sport. Incorporating targeted exercises into your routine is key to building strength and resilience. Strengthening the muscles surrounding the knees and ankles through exercises such as lunges and calf raises enhances stability, reducing the risk of sprains and strains. Core exercises contribute to overall body balance, promoting a more efficient running gait. Flexibility exercises, such as dynamic stretches, help improve the range of motion and minimize the impact on joints. Regular strength training sessions, focusing on both the upper and lower body, foster muscular endurance that is vital for sustained running performance. Listening to your body, incorporating adequate rest, and gradually increasing mileage are essential components of injury prevention. If you are seeking more information about how running injuries may affect the feet, in addition to learning about effective prevention methods, it is suggested that you schedule an appointment with a podiatrist.
Exercising your feet regularly with the proper foot wear is a great way to prevent injuries. If you have any concerns about your feet, contact Dr. Alan J. Spector of Shore Podiatry. Our doctor will treat your foot and ankle needs.
How to Prevent Running Injuries
Many common running injuries are caused by overuse and overtraining. When the back of the kneecap starts wearing out and starts causing pain in your knee, this is commonly referred to as runner’s knee. Runner’s knee is a decrease in strength in your quadriceps and can occur if you’re not wearing properly fitted or supporting shoes. To prevent runner’s knee, focusing on hip strengthening is a good idea, as well as strengthening your quads to keep the kneecaps aligned.
What Are Some Causes of Running Injuries?
- One cause of a common running injury is called iliotibial band syndrome.
- Plantar fasciitis is also another common injury.
- Stress fractures can occur from overtraining, lack of calcium, or even your running style.
Best Ways to Prevent Running Injuries
- Wear footwear that fits properly and suits your running needs.
- Running shoes are the only protective gear that runners have to safeguard them from injury.
- Make a training schedule. Adding strengthening exercises as well as regular stretching can help keep you strong and limber and can lessen the possibility of injuries.
- Stretching keeps muscles limber; this will help you gain better flexibility.
If you have any questions please feel free to contact our office located in Point Pleasant, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Overtraining and overusing the feet are the main causes of common running injuries. A number of these common injuries are caused by overrunning. Runner’s knee is a condition that is characterized by the back of the kneecap beginning to wear away and cause pain in the knee. This frequently occurs due to either a decrease in strength in the quadriceps muscles or ill-fitting shoes that are lacking in proper support for the inside of the forefoot. Strengthening exercises focusing on the quad muscle and sports orthotics are the usual treatments for those suffering from runner’s knee. Prevention of the condition lies in a focus on hip strengthening and quad-strengthening to keep the kneecap aligned. To help learn the best exercise to heal runner’s knee, one can also undergo physical therapy.
One common injury, called iliotibial band syndrome, is often caused by overtraining. This condition occurs when the iliotibial band gets irritated, creating pain and discomfort in the outside knee area. Plantar fasciitis, another common running injury, also occurs as a result of inflammation and irritation. Plantar fasciitis is an inflammation and irritation of the bone in the foot. A large amount of pain is often experienced due to plantar fasciitis. The condition can be caused by a high arch, improper footwear, tight muscles, or flat feet. It can best be avoided by stretching and wearing appropriate footwear that supports the foot.
Another common injury for runners is stress fractures. These injuries occur due to running style, overtraining, or a lack of calcium. Stress fractures most often occur in several locations in runners, including the inner bone of the leg, the thighbone, the bone at the base of the spine and the bones of the toes. Stress fractures are best prevented by wearing proper footwear and by running on flat and hard surfaces; this will absorb some of the shock created during running.
Aside from overtraining, other causes of common running injuries include ill-fitting footwear, a lack of flexibility and strength, and irregular biomechanics. The best way to avoid running injuries is to prevent them from even occurring. Both iliotibial band syndrome and stress fractures are preventable. The first step that should be taken to prevent running injuries is to only wear footwear that fits properly and that is appropriate for whatever activity you are doing. Running shoes are the only protective gear available to runners that can safeguard them from sustaining injuries. Choosing the right pair of shoes is therefore extremely important. While running shoes are an important factor, it is also important to consider other facets of your running routine such as training schedules, flexibility, and strengthening. These elements should be considered and altered according to your running needs to best maximize your run and minimize the possibility of injury. Careful stretching before and after a run should also be considered to help prevent running injuries. Stretching muscles enables greater flexibility and a lesser chance of sustaining injury.

Managing persistent foot pain or deformities can be challenging, often prompting the consideration of foot surgery when conservative treatments prove ineffective. In such cases, surgery becomes a viable option. Bunions, or hallux valgus, can be surgically managed when conservative treatments fail to alleviate pain and hinder day-to-day functioning. Similarly, hammertoes may necessitate surgery when they become rigid and painful, causing issues such as inflammation and open wounds. Metatarsal surgery addresses various foot issues caused by conditions like rheumatoid arthritis, fractures, and dislocated joints. Ankle osteoarthritis, marked by symptoms such as pain, stiffness, and swelling, may require surgical intervention. Achilles tendon disorders, including tendonitis, may prompt surgery consideration. Morton's neuroma, characterized by nerve thickening between the third and fourth toes, might necessitate surgery for those unresponsive to non-surgical management. Posterior tibial tendon dysfunction, or adult-acquired flatfoot, may require surgical intervention as symptoms worsen, aiming to restore the function of the posterior tibial tendon and support the arch. Foot surgery is generally considered a last resort, but it can be a consideration when conservative treatments no longer provide relief for persistent foot pain or deformities. It is suggested that if you are suffering from continual foot, toe, or ankle pain that you schedule an appointment with a podiatrist to determine whether surgery is the appropriate course of action for you.
Foot surgery is sometimes necessary to treat a foot ailment. To learn more, contact Dr. Alan J. Spector of Shore Podiatry. Our doctor will assist you with all of your foot and ankle needs.
When Is Surgery Necessary?
Foot and ankle surgery is generally reserved for cases in which less invasive, conservative procedures have failed to alleviate the problem. Some of the cases in which surgery may be necessary include:
What Types of Surgery Are There?
The type of surgery you receive will depend on the nature of the problem you have. Some of the possible surgeries include:
Benefits of Surgery
Although surgery is usually a last resort, it can provide more complete pain relief compared to non-surgical methods and may allow you to finally resume full activity.
Surgical techniques have also become increasingly sophisticated. Techniques like endoscopic surgery allow for smaller incisions and faster recovery times.
If you have any questions please feel free to contact our office located in Point Pleasant, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
When conservative, noninvasive methods prove ineffective, surgery may be selected as the next course of action for the treatment of your foot or ankle condition. A wide number of foot and ankle surgical procedures exist, and it is up to your podiatrist to determine which intervention will be most appropriate and helpful for your case. Some surgical procedures include bunion surgery, fusion, hammertoe surgery, heel spur surgery, metatarsal surgery, nail surgery, neuroma surgery, reconstructive surgery, skin surgery, and tendon surgery. Typically, surgery is turned to as a definitive way to alleviate excessive pain or discomfort and to return your foot to full mobility.
Regardless of the location on the body, all surgical procedures require preoperative testing and examination to ensure the surgery’s success and preferred outcome. A review of your medical history and medical conditions will take place, as will an evaluation of any current diseases, illnesses, allergies, and medications. Tests such as blood studies, urinalyses, EKG, X-rays, and blood flow studies may be ordered. Because the procedure involves the foot and/or ankle, the structures of your feet while walking may also be observed by your podiatrist.
Care post-surgery will depend on the type of surgical procedure performed. Typically, all postoperative care involves rest, ice, compression, and elevation. To improve and ensure a safe recovery, your foot and ankle surgeon may also employ the use of bandages, splints, surgical shoes, casts, crutches, or canes. He will also determine if and when you can bear weight. A timely and thorough recovery is a priority for both you and your podiatrist, and carefully following postoperative instructions can help achieve this.

One of the most common indicators of a fractured heel bone is tenderness in the area that causes pain, even with slight pressure. Swelling in the foot and ankle area is another prevalent symptom, often accompanied by visible bruising. Individuals with heel fractures usually find it impossible to bear weight on the affected foot, leading to significant mobility limitations. The diagnosis of heel bone fractures typically involves X-rays and computed tomography, or CT, scans. X-rays can provide a clear image of the injury, but in more complex cases, CT scans may be used to obtain a detailed, three dimensional view of the affected area. Non surgical treatment involves protecting the fractured area with a splint, resting the foot by avoiding weight-bearing, and using crutches. Once swelling subsides, a podiatrist may apply a cast to stabilize the fracture. Surgical intervention may be necessary when the fracture affects the joint. It is important to avoid putting any weight on the injured heel until the fracture has fully healed, which may take several months. If you believe you have fractured your heel bone, it is suggested that you make an appointment with a podiatrist.
Many people suffer from bouts of heel pain. For more information, contact Dr. Alan J. Spector of Shore Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our office located in Point Pleasant, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Have you ever gotten up from a chair or out of bed in the morning, and upon taking that first step, feel like your heel has stepped on a tack? Many people experience a feeling of sharp pain which radiates into their arch from their heel and which does not allow them to put their heel on the floor. Sometimes they need to sit back down, stand only on their toes and use the wall for balance. If you can take a few steps, it seems to go away and lessen, allowing you to then resume your activity. Later, throughout your day and after a period of rest, it can happen again. If this sounds familiar you may be suffering from your first attack of heel pain.
Heel pain is a debilitating condition that affects day to day activities. Running and walking both causes stress on the heel because the heel is the part of the foot that hits the ground first. This means that the heel is taking on your entire weight. Diagnosis and treatments for heel pain can be easily found through your podiatrist.
Plantar Fasciitis
One of the main causes of heel pain is a condition known as plantar fasciitis. The plantar fascia is a band of tissue that extends along the bottom of the foot, from the toe to the bottom of the heel. A rip or tear in this ligament can cause inflammation of these tissues, resulting in heel pain. People who do not wear proper fitting shoes are often at risk of developing problems such as plantar fasciitis. Unnecessary stress from ill-fitting shoes, weight change, excessive running, and wearing non-supportive shoes on hard surfaces are all causes of plantar fasciitis.
Achilles Tendonitis
Achilles tendonitis is another cause of heel pain. Similar to plantar fasciitis, inflammation of the Achilles tendon will cause heel pain due to stress fractures and muscle tearing. A lack of flexibility of the ankle and heel is an indicator of Achilles tendonitis. If left untreated, this condition can lead to plantar fasciitis and cause even more pain on your heel.
Heel Spur
A third cause of heel pain is a heel spur. A heel spur occurs when the tissues of the plantar fascia undergo a great deal of stress, leading to a separation of the ligament from the heel bone entirely. This results in a pointed fragment of bone on the ball of the foot, known as a heel spur.
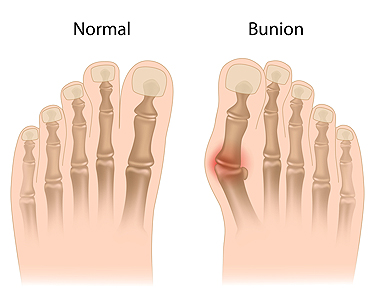
A bunion, medically termed hallux valgus, is a prominent, bony protrusion at the base of the big toe. Often, the only indicator of a mild bunion is its physical manifestation. However, it can also result in discomfort, swelling, and alterations in the foot's structure. In extreme instances, surgical intervention might be necessary due to related issues. Key visual indicators of a bunion are the big toe deviating toward the other toes, forming an outward bulge on the first foot bone. Additionally, there may be a raised bony bump on the foot's exterior, tough skin under the big toe, and calluses on the adjacent toe. Over time, the foot's form may drastically change, impacting both the big toe and other foot regions, making shoe selection challenging. Resulting structural modifications can cause pain, swelling, and bursitis, which is an inflammation of the toe joint's cushioning sac. Some people may face mobility issues with their big toe, affecting their walking. While many individuals do not encounter severe problems from bunions, if left untreated, complications such as arthritis in the big toe or deformities in the adjacent toe can arise. If you have a painful bunion, it is suggested that you make an appointment with a podiatrist who can intervene and help prevent severe complications.
If you are suffering from bunions, contact Dr. Alan J. Spector of Shore Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
If you have any questions, please feel free to contact our office located in Point Pleasant, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.